Treatment of acute acromioclavicular joint dislocations type III and type V by Rockwood classification using a dynamic stabilization system under arthroscopic control with and without suture
Serhii Bezruchenko, Oleksii Dolhopolov
Summary. Acute acromioclavicular (AC) joint dislocation is still a challenging task for orthopedic surgeons.
Objective: to compare the clinical and radiological results of treatment of patients with acute dislocation of the acromial end of the clavicle who were treated with a dynamic stabilization system with and without suture of acromioclavicular ligaments under arthroscopic control.
Materials and Methods. A retrospective analysis of the treatment of 44 patients with acute AC joint dislocations type III and type V by Rockwood classification was performed. The patients were divided into 2 groups: group I – 18 patients (40.9%) who underwent stabilization of the dislocation and fixation of the acromial end of the clavicle using a dynamic stabilization system and suture of the ligaments of the acromioclavicular joint under arthroscopic control; group II – 26 patients (59.1%) who underwent stabilization of the dislocation and fixation of the acromial end of the clavicle using a dynamic stabilization system without suture of the ligaments of the acromioclavicular joint under arthroscopic control. There were 40 male (90.9%) and 4 female (9.1%) patients aged 18–58 years (mean age 32.9±10.1 years). The mean time from injury to surgical treatment was 8.3±3.2 days (from 3 to 17 days). Clinical observation was carried out at an average time of 20.1±3.9 months after surgery (from 12 to 28 months). Clinical outcomes were assessed using the Oxford Shoulder scale, the Constant-Murley scale, and the Acromioclavicular Joint Instability Scoring System.
Results. The mean Oxford Shoulder score at the final follow-up on the injured side was 45.8±1.3 points and 46.2±1.3 points (p=0.422) in groups I and II, respectively. The mean Constant-Murley score at the final follow-up on the injured side was 94.6±2.4 points and 91.7±4.2 points (p=0.0134) in groups I and II, respectively. The mean score on the Acromioclavicular Joint Instability Scoring System at the final follow-up on the injured side was 83.8±7.1 points and 78.1±11.8 points (p=0.075) in groups I and II, respectively. No significant complications were observed in both groups.
Conclusions. The combination of the arthroscopically assisted technique of reconstruction of the acromioclavicular ligaments using high-strength sutures and fixation of the coracoclavicular ligaments using a dynamic stabilization system provides good long-term clinical results.
Key words: acromioclavicular joint; dislocation; horizontal instability; acute dislocation.
Introduction
Acute acromioclavicular (AC) joint dislocation is commonly seen in shoulder injuries in active individuals and accounts for from 9% to 12% of shoulder girdle injuries [1]. Many AC joint reconstruction techniques have been developed over the years. There are more than 162 surgical techniques to treat acromioclavicular joint dislocation [2]. Arthroscopically assisted anatomic reconstruction of the AC joint is a technically challenging procedure. Deficient superior and posterior AC ligaments healing may contribute to persistent horizontal AC joint instability, which is reported in up to 50% of patients following arthroscopic reconstruction of AC joint dislocations. Modern techniques employ additional synthetic AC stabilization consisting of high-strange absorbable or non-absorbable cerclages, anchors techniques, and a combination of techniques [3]. Biomechanical studies have shown that a combination of restoration both superior-inferior stabilization (coracoclavicular ligaments) and anterior-posterior stabilization (acromioclavicular ligaments) of the AC joint enables restoration of physiological stability [4]. Saier T et al. demonstrated in an experiment that only a combination of anatomical repair of AC ligaments can adequately reestablish physiological horizontal stability in acute AC joint dislocation [5]. The rate of complications after arthroscopically assisted AC joint reconstruction and stabilization is high and varies from 12.5% to 27.1%, and can reach 40% [6, 7]. Siva Thangaraju et al. showed a high-rate traumatic periimplant fracture 2 years post-operatively after arthroscopically assisted AC joint reconstruction [8].
Surgical treatment of AC joint dislocation has changed extremely in the last decade since the advent of arthroscopically assisted techniques. Postoperative failures and complications still are common after AC joint dislocation treatment. The incidence of these complications varies by reconstructive technique, as well as by study.
The aim of this study is an analysis of the clinical and radiographic outcomes and complications in patients with acute AC joint dislocation who were treated with arthroscopically assisted stabilization technique using a dynamic stabilization system with and without AC ligaments cerclage.
Materials and Methods
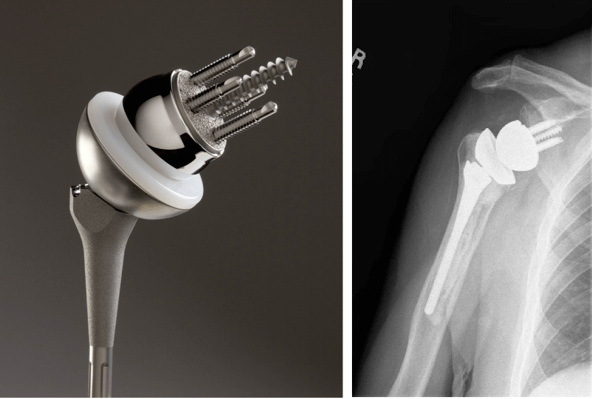
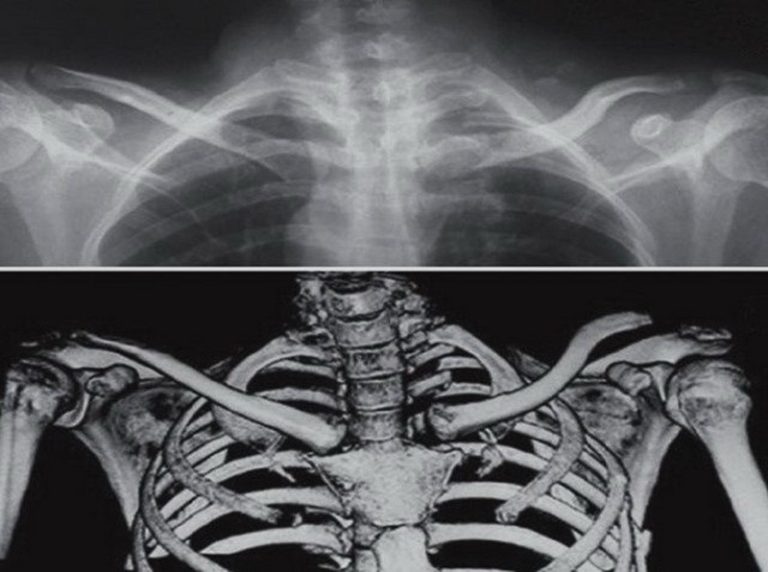
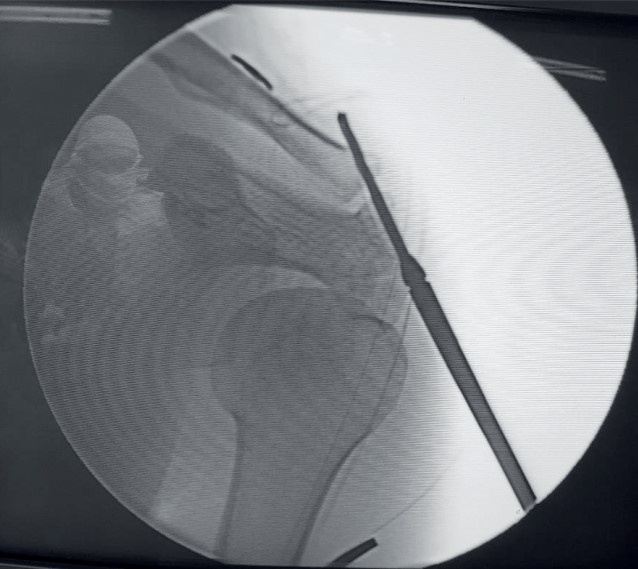
A retrospective review of 44 patients with acute AC joint dislocations type III and type V by Rockwood classification, who were treated at the Department of Microsurgery and Reconstructive-Recovery Surgery of the Upper Limb (SI “Institute of Traumatology and Orthopedics of NAMS of Ukraine”) between January 2014 and July 2019, was performed. The patients were divided into 2 groups. Group I included 18 patients (40.9%) who underwent arthroscopically assisted stabilization of AC joint dislocation with a dynamic stabilization system (Dog Bone®, Arthrex, Inc) and AC ligaments cerclage using #2 FiberTape® (Arthrex, Inc) (Fig. 1, 2). Group II included 26 patients (59.1%) who underwent arthroscopically assisted stabilization of acute AC joint dislocation with a dynamic stabilization system (Dog Bone®, Arthrex, Inc) without AC joint ligaments suture (Fig. 3). There were 40 male (90.9%) and 4 female (9.1%) patients aged 18–58 years (mean age 32.9±10.1 years). The mean time from injury to surgical treatment was 8.3±3.2 days (from 3 to 17 days). The included criteria were acute AC joint dislocations (less than 3 weeks) type III and type V by Rockwood classification. The exclusion criteria were existing history of bone disease, combined fracture of the clavicle, scapula, humerus, or another concomitant shoulder injury.
All patients were examined using clinical and instrumental methods of diagnostics: cross-body adduction test, O`Brien active compression test, AC resisted extension test, X-ray examination in Zanca view, axial view and Alexander view, and ultrasound examination with a functional probe [9].
Dynamical AC joint instability examinations were performed by ultrasound examination in the frontal, axial, and sagittal projections at final follow-up after surgical treatment. Vertical instability was identified in frontal projection: we determined the distance between the upper border of the acromial process and the upper border of the acromial end of the clavicle on the side of the injury. Additionally, a provocative test was performed – the distance between the upper border of the acromial process and the upper border of the acromial end of the clavicle on the side of the injury was measured during the “piano key” test. Horizontal instability of the AC joint was identified in the axial projection; we determined the distance from the anterior border of the acromial process to the anterior border of the acromial end of the clavicle on the side of injury. Additionally, a provocative test was performed – the distance from the anterior border of the acromial process to the anterior border of the acromial end of the clavicle on the side of the injury was measured during the Paxinos test. In the sagittal projection, we determined coracoclavicular (CC) distance – between the most superior border of the coracoid process and the inferior border of the clavicle on the injured side [10, 11].
In all patients, clinical final follow-up outcomes were assessed by Oxford Shoulder scale [12], Constant-Murley scale [13], and Acromioclavicular Joint Instability Scoring System [14]. These assessments were performed at a mean of 20.1±3.9 months after surgical treatment (from 12 to 28 months).
After the surgery, the arm was supported with a sling for 5 weeks. During this time, only active motions in the elbow and wrist were allowed (three times a day for 10 minutes each time). Progressive rehabilitation was initiated after 5 weeks. During weeks 6-12, a full range of motions was allowed, as well as isometric muscle strengthening. Strengthrelated activities were added after 12 weeks.
Statistical analysis was performed using the STATISTICA 12.0 (StatSoft Inc. USA) and Microsoft Excel. Descriptive statistics, Student’s t-test, and the Mann-Whitney U-test were used to determine outcome differences between the two treatment groups. The level of statistical significance of p<0.05 was considered.
Results
A total of 44 patients were included in this study: group I − 10 patients with type III and 8 patients with type V; group II − 13 patients with type III and 13 patients with type V by Rockwood classification (p=0.724). The mean final follow-up period was 20.6±3.8 months in group І and 19.8±4.2 months in group ІІ (р=0.516). The mean age was 35.8±9.6 years in group I and 30.8±10.1 years in group II (р=0.111). There were 16 males and 2 females in group I and 24 males and 2 females in group II (p=0.706). The mean time from injury to surgical treatment was 8.4±3.6 days in group I and 8.3±3.1 days in group II (р=0.905). The right side was affected in 32 patients (72.7%).
The mean Oxford Shoulder score at the final followup on the injured side was 45.8±1.3 points and 46.2±1.3 points (p=0.422), on the healthy side − 46.3±0.9 points and 46.4±1.0 points (p=0.965) in groups I and II, respectively. This difference with the healthy side after surgical treatment was statistically significant (p>0.05).The mean Constant-Murley score at the final followup on the injured side was 94.6±2.4 points and 91.7±4.2 points (p=0.0134), on the healthy side − 96.3±1.3 points and 96.8±1.6 points (p=0.301) in groups I and II, respectively. This difference with the healthy side after surgical treatment was not statistically significant (p<0.05).
The mean score by the Acromioclavicular Joint Instability Scoring System at the final follow-up on the injured side was 83.8±7.1 points and 78.1±11.8 points (p=0.075), on the healthy side − 93.1±2.7 points and 93.4±2.7 points (p=0.613) in groups I and II, respectively. This difference with the healthy side after surgical treatment was not statistically significant (p<0.05).
The final follow-up ultrasound examination was performed in 44 patients (Table 1).
Intra-articular pathology was diagnosed and treated arthroscopically in 11 patients (61.1%) in group I: 7 patients (38.9%) with SLAP lesions, 2 patients (11.1%) with rotator cuff tears, 3 patients (16.7%) with pulley lesion tear, and 1 patient (5.6%) with intra-articular loose bodies. In group II, intra-articular pathology was diagnosed in 14 patients (53.8%): 10 patients (38.5%) with SLAP lesions, 3 patients (11.5%) with rotator cuff tears, and 6 patients (23.1%) with pulley lesion tear.
There were no major complications such as a fracture of the clavicular, coracoid process or acromion process around the implant, hardware failure, implant migration, or deep infection. Group I included 2 patients with vertical instability in Zanca view and horizontal instability in Alexander view, 3 patients with CC ossification, 2 patients with osteolysis of acromial end of the clavicle, 2 patients with posttraumatic osteoarthritis of the AC joint, and 1 patient with intra-articular loose bodies. Group II included 6 patients with a vertical subluxation in Zanca view, 9 patients with horizontal instability in Alexander view, 5 patients with posttraumatic osteoarthritis of the AC joint, 5 patients with osteolysis of the acromial end of the clavicle, 2 patients with lateral mobilization, and 1 patient with medal mobilization of coracoid Dog Bone button without clinically worse results.
Discussion
The arthroscopically assisted reconstruction of acute AC joint dislocation is a minimally invasive method of restoration of coracoclavicular ligaments, which has become more popular in recent years. This technique was first described with the use of a single implant, but a high rate of early complications (suture breakage, unsatisfactory radiographic result, and coronoid fracture) subsequently switched to the double dynamic stabilization system technique of restoration of conoid and trapezoid ligament to avoid vertical and horizontal instability of the AC joint. Markus Scheibel et al. presented the combined arthroscopically assisted double TightRope technique, which represents a safe technique with good and excellent early clinical results in the presence of partial recurrent vertical and horizontal AC joint instability [14]. In 2019, Markus Scheibel et al. described a new arthroscopically assisted technique with one low-profile implant (TightRope and Dog Bone, Arthrex, Inc) for vertical stability and acromioclavicular cerclage with non-absorbable tape for horizontal stabilization. This low-profile device is self-tensioning and facilitate a simplified anatomical reduction process [15]. Thibault Lafosse et al. described the all-arthroscopic technique that enables true sutures of the CC ligaments, which are loaded with a tape and reattached to the lower surface of the clavicle, so potential healing is thereby improved [16]. Abdul-Ilah Hachem et al. provided the same technique of arthroscopically assisted single-tunnel coracoclavicular fixation using 2 buttons and FiberTape
Table 1. Ultrasound examination of AC joint at the final follow-up

Cerclage sutures (Arthrex, Naples, FL) associated with a minimally invasive percutaneous AC fixation in a transosseous figure-of-eight configuration of the FiberTape for the comprehensive treatment of unstable AC joint dislocations [17].
The present study shows the results of treatment of acute acromioclavicular joint dislocations type III and type V by Rockwood classification with arthroscopically assisted technique using a dynamic stabilization system with and without AC ligaments suture. We have found that clinical and radiographic results in patients with acute AC joint dislocation type III by Rockwood classification with #2 FiberTape® (Arthrex, Inc) and without AC ligaments suture were statistically significant (p>0.05) and have minimum postoperative instability – 2 patients with vertical instability in Zanca view and horizontal instability in Alexander view. However, clinical and radiographic results were not statistically significant (p<0.05) in patients with acute AC joint dislocation type V by Rockwood classification; there were 6 patients with a vertical subluxation in Zanca view and 9 patients with horizontal instability in Alexander view.
Ultrasound is a valuable diagnostic and very sensitive method for displaying injury and dynamic examination of the horizontal and vertical instability of the AC joint. In this study, an ultrasound examination was performed at the final follow-up; in patients with type III by Rockwood classification, the difference between the groups with and without AC cerclage was statistically significant, but clinical and radiographic outcomes were the same in both groups. In patients with type V by Rockwood classification, AC joint dislocation difference between the groups with and without AC cerclage was not statistically significant; clinical and radiographic outcomes were worse in group II, and rates of complications – subluxation in Zanca view (vertical instability) and in Alexander view (horizontal instability) – were higher in group II (p>0.05).
Finally, a limitation of this study is that horizontal and vertical instability are more often associated with hightype AC joint dislocation. Thus, dynamic anterior-posterior horizontal instability in patients with AC joint dislocation type V by Rockwood classification plays a major role in inferior clinical results.
Conclusions
The combination of arthroscopically assisted technique of acromioclavicular ligaments reconstruction using high-strength sutures and coracoclavicular ligaments with dynamic stabilization system provides good clinical and radiological results, as well as minimized vertical and horizontal instability in the postoperative period.
Conflict of interest. The author declare no conflict of interest. This publication has not been, is not, and will not be the subject of commercial interest in any form.

Fig. 1. Step of acromioclavicular cerclage (model): A – navigation system for drill through lateral end of the clavicle, B – 3.0-mm cannulated drill is passed through the lateral end of the clavicle; C, D, E – navigation and 3.0-mm cannulated drill is passed through the acromion process, F – final view of coracoclavicular and acromioclavicular cerclages

References
1. van Bergen CJA, van Bemmel AF, Alta TDW, van Noort A. New insights in the treatment of acromioclavicular separation. World J Orthop. 2017 Dec 18;8(12):861-873. DOI: 10.5312/wjo.v8.i12.861; PMID: 29312844; PMCID: PMC5745428.
2. Allemann F, Halvachizadeh S, Waldburger M, Schaefer F, Pothmann C, Pape HC, et al. Different treatment strategies for acromioclavicular dislocation injuries: a nationwide survey on open/minimally invasive and arthroscopic concepts. Eur J Med Res. 2019 Mar 23;24(1):18. DOI: 10.1186/s40001-019-0376-7; PMID: 30904018; PMCID: PMC6431035.
3. Maier D, Jaeger M, Reising K, Feucht MJ, Südkamp NP, Izadpanah K. Injury patterns of the acromioclavicular ligament complex in acute acromioclavicular joint dislocations: a cross-sectional, fundamental study. BMC Musculoskelet Disord. 2016 Sep 6;17(1):385. DOI: 10.1186/s12891-016-1240-3. PMID: 27600992; PMCID: PMC5012011.
4. Wylie JD, Johnson JD, DiVenere J, Mazzocca AD. Shoulder Acromioclavicular and Coracoclavicular Ligament Injuries: Common Problems and Solutions. Clin Sports Med. 2018 Apr;37(2):197-207. DOI: 10.1016/j.csm.2017.12.002; PMID: 29525023.
5. Saier T, Venjakob AJ, Minzlaff P, Föhr P, Lindell F, Imhoff AB, et al. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2015 May;23(5):1498-505. DOI: 10.1007/s00167-014-2895-7; PMID: 24554242.
6. Martetschläger F, Horan MP, Warth RJ, Millett PJ. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013 Dec;41(12):2896-903. DOI: 10.1177/0363546513502459; PMID: 24007761.
7. Clavert P, Meyer A, Boyer P, Gastaud O, Barth J, Duparc F; SFA. Complication rates and types of failure after arthroscopic acute acromioclavicular dislocation fixation. Prospective multicenter study of 116 cases. Orthop Traumatol Surg Res. 2015 Dec;101(8):313-6. DOI: 10.1016/j.otsr.2015.09.012; PMID: 26545944.
8. Thangaraju S, Tauber M, Habermeyer P, Martetschläger F. Clavicle and coracoid process periprosthetic fractures as late post-operative complications in arthroscopically assisted acromioclavicular joint stabilization. Knee Surg Sports Traumatol Arthrosc. 2019 Dec;27(12):3797-802. DOI: 10.1007/s00167-019-05482-7; PMID: 30900030.
9. Rockwood CJ, Wirth MA, Fehringer EV, Matsen FA, Sperling JW, Lippitt SB. Rockwood and matsen’s the shoulder, fifth edition 5th ed. Philadelphia, PA: Elsevier; 2018. 379-398 p.
10. Hobusch GM, Fellinger K, Schoster T, Lang S, Windhager R, Sabeti-Aschraf M. Ultrasound of horizontal instability of the acromioclavicular joint: A simple and reliable test based on a cadaveric study. Wien Klin Wochenschr. 2019 Feb;131(3-4):81-86. DOI: 10.1007/s00508-018-1433-x; PMID: 30617708; PMCID: PMC6394808.
11. Faruch Bilfeld M, Lapègue F, Chiavassa Gandois H, Bayol MA, Bonnevialle N, Sans N. Ultrasound of the coracoclavicular ligaments in the acute phase of an acromioclavicular disjonction: Comparison of radiographic, ultrasound and MRI findings. Eur Radiol. 2017 Feb;27(2):483-90. DOI: 10.1007/s00330-016-4413-4; PMID: 27236814.
12. Dawson J, Rogers K, Fitzpatrick R, Carr A. The Oxford shoulder score revisited. Arch Orthop Trauma Surg. 2009 Jan;129(1):119-23. DOI: 10.1007/s00402-007-0549-7; PMID: 18183410.
13. Constant CR, Gerber C, Emery RJ, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008 Mar-Apr;17(2):355-61. DOI: 10.1016/j.jse.2007.06.022; PMID: 18218327.
14. Scheibel M, Dröschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011 Jul;39(7):1507-16. DOI: 10.1177/0363546511399379; PMID: 21436458.
15. Minkus M, Maziak N, Moroder P, Scheibel M. Arthroscopic low-profile reconstruction for acute acromioclavicular joint instability. Obere Extremität. 2019 Feb;14(6):60-65. DOI: 10.1007/s11678-019-0506-4.
16. Lafosse T, Fortané T, Lafosse L. All-Endoscopic Treatment of Acromioclavicular Joint Dislocation: Coracoclavicular Ligament Suture and Acromioclavicular Ligament Desincarceration. Arthrosc Tech. 2020 Sep 25; 9(10):e1485-e1494. DOI: 10.1016/j.eats.2020.06.011; PMID: 33134050; PMCID: PMC7587138.
17. Hachem AI, S RR, Costa G, Verdalet I, Ezzeddine H, Rius X. Arthroscopically Assisted Comprehensive Double Cerclage Suture Fixation Technique for Acute Acromioclavicular Joint Separation. Arthrosc Tech. 2020 Sep 15;9(10):e1495-e1504. DOI: 10.1016/j.eats.2020.06.012; PMID: 33134051; PMCID: PMC7587229.
Лікування травматичних вивихів акроміально-ключичного суглоба III та V типу за класифікацією Rockwood за допомогою динамічної системи стабілізації під артроскопічним контролем з та без шва зв’язок акроміально-ключичного суглоба
Serhii Bezruchenko, Oleksii Dolhopolov
Резюме. Травматичні вивихи акроміального кінця ключиці і дотепер є складними в лікуванні для лікарів травматологів-ортопедів.
Мета. Порівняти клінічні та радіографічні результати лікування хворих із травматичним вивихом акроміального кінця ключиці, для лікування яких було використано метод динамічної системи стабілізації з та без шва акроміально-ключичних зв’язок під артроскопічним контролем.
Матеріали і методи. Проведено ретроспективний аналіз лікування 44 пацієнтів із травматичним вивихом акроміального кінця ключиці III та V типу за класифікацією Rockwood. Хворі були розподілені на 2 групи: I група – 18 пацієнтів (40,9%), яким було виконано усунення вивиху та фіксація акроміального кінця ключиці з використанням динамічної системи стабілізації та шов зв’язок акроміально-ключичного суглоба під артроскопічним контролем; II група – 26 пацієнтів (59,1%), яким було виконано усунення та фіксація вивиху акроміального кінця ключиці з використанням динамічної системи стабілізації без шва зв’язок акроміально-ключичного суглоба під артроскопічним контролем. Серед них було 40 чоловіків (90,9%) та 4 жінки (9,1%), середній вік яких становив 32,9±10,1 року (від 18 до 58 років). Середній термін від моменту травми до оперативного лікування складав 8,3±3,2 доби (від 3 до 17 днів). Клінічне спостереження проводили в середній термін 20,1±3,9 місяця після оперативного лікування (від 12 до 28 місяців). Оцінка клінічних результатів проводилась за допомогою шкали Oxford Shoulder, шкали Constant-Murley та шкали Acromioclavicular Joint Instability Scoring System.
Результати. Середній бал за шкалою Oxford Shoulder під час остаточного спостереження склав 45,8±1,3 бала та 46,2±1,3 бала (p=0,422) в I та II групах відповідно. Середній бал за шкалою Constant-Murley під час остаточного спостереження склав 94,6±2,4 бала та 91,7±4,2 бала (p=0,0134) в I та II групах відповідно. Середній бал за шкалою Acromioclavicular Joint Instability Scoring System під час остаточного спостереження склав 83,8±7,1 бала та 78,1±11,8 бала (p=0,075) в I та II групах відповідно. В обох групах значних ускладнень виявлено не було.
Висновки. Поєднання артроскопічної асистованої техніки реконструкції акроміально-ключичних зв’язок надміцним шовним матеріалом та фіксація дзьобоподібно-ключичних зв’язок із застосуванням динамічної системи стабілізації забезпечує хороші віддалені клінічні результати.
Ключові слова: акроміально-ключичний суглоб; вивих; горизонтальна нестабільність; травматичний вивих.